Embedded in the Dash concept were a couple of assumptions that I thought needed exploration:
-
Patients don't report relapses because of the burdens of doctor visits and the ensuing approval process for treatment
-
Patients don't report relapses because they are too physically and cognitively incapacitated to do so
We needed to look more closely at the point of relapse and what was happening at this moment.
Research subject:
MS patients' decision making processes at point of relapse
Research statement:
We want to discover how MS patients make decisions about their condition during a relapse so our brand can appropriately support patients in getting treatment.
Learning goals:
- Discover what a relapse means to MS patients physically and emotionally
- Discover patient needs and desired outcomes when experiencing a relapse
- Learn about barriers to those desired outcomes, and barriers to taking action on their condition during a relapse
- Understand how they view MS treatment, and why they view it that way
I proposed doing one on one interviews with MS patients. We would run interactive mapping and collaging where patients could take us through a relapse, mapping out their actions and emotions with drawing materials and object prompts. This could open up recollections of a past relapses where trauma may have clouded memory, and facilitate descriptions of complex emotions.
I looked forward to the rich descriptions and how that would build empathy among our all our internal specializations and the client, and then how the artifacts would lead to rich discussions after the interviews were done.
However, the client had lots of heart for the Dash concept. With the team sold on this idea, I had to pivot the research so that a concept prototype would be tested. My goal was to execute a usability test but also use the app as a stimulus for participant descriptions of complex emotions and behaviors.
Revised Research subject:
MS patients' interactions with the Dash app
Revised Research statement:
We want to learn if our concept of the Dash app meets patient needs during a relapse and how they can use it to take action on their condition
Revised Learning goals:
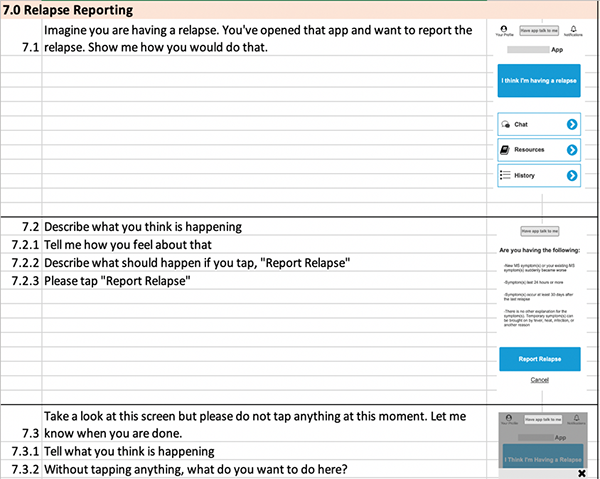
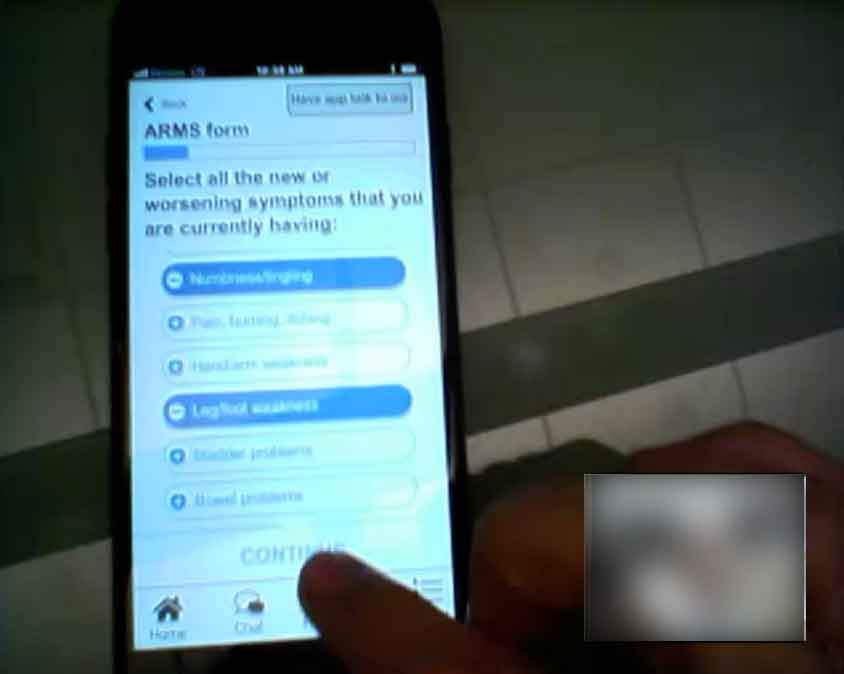
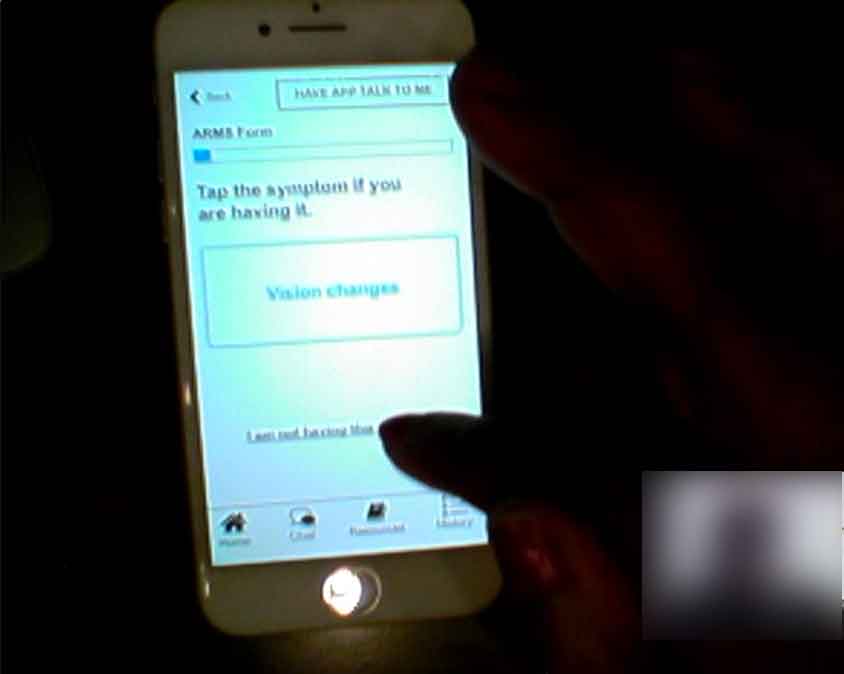
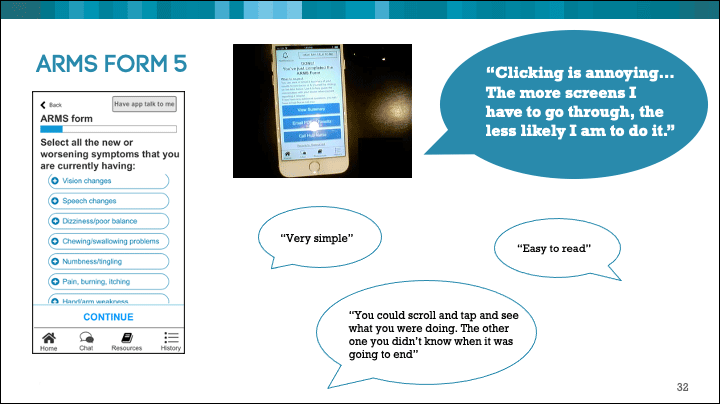
- Evaluate the design and flow of the app to learn if participants understand how to use it
- Evaluate the content and features of the app to see if it meets patient needs
- Uncover pain points during an MS relapse
The team agreed to a hybrid of open ended questioning and usability testing. We tested an Axure prototype, running the in-person interviews with Morae.